What Should Be The Number One Priority for The US Health Care System
On the front page of this blog-post website I list what the priorities are for Health Care Systems in the US. I didn’t poll anyone. I didn’t have to. I’ve lived it for 40 years. In case you can’t recall the list, here it is:
- Money – Profit, Margin (even if they are “not for profit”)
- Growth – more opportunity for revenue = more profit potential
- Patient Satisfaction – this is based on niceties, not clinical (I have a pretty hospital room, for example)
- Clinical Quality -you getting the best care possible
- Employee Satisfaction – includes the physicians and APCs who have privileges at the hospitals
- Charity/uninsured care – the reluctance to have to negatively affect the health care system’s profit margin for these folks
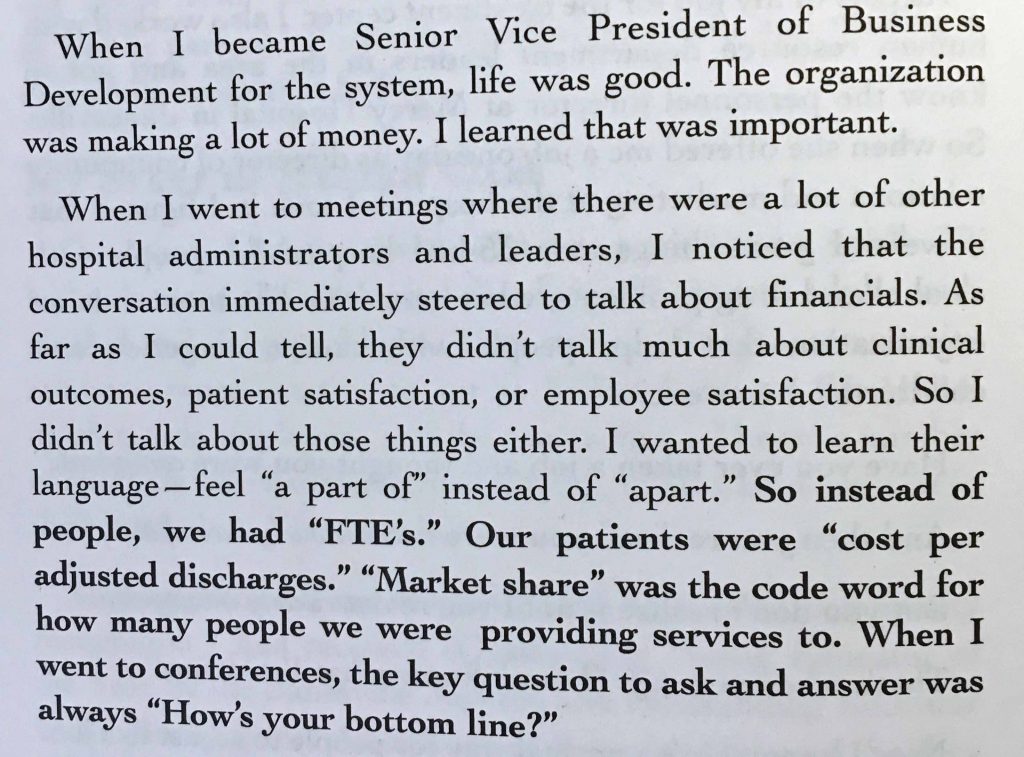
A lot of my previous posts relate data, literature and personal experiences that support my list. And, if you don’t believe my list, maybe you’ll believe Quint Studer, who was President of Baptist Hospital when they won a Malcolm Baldrige Award. FYI, Quint got his masters degree in Special Education, not an MBA. Maybe that’s why he was so good (refer to my post “Why It Is So Difficult for Health Care Systems to Perform to Expectations”). And, so you won’t think I paraphrased or altered Quint’s writing in his book “Hardwiring Excellence” here is a photo of the page for you to read:
So, what should be the number one priority for a health care organization or person? Do I really have to ask?
It should be YOU, the patient!! Of course!
If it were you that was the number one priority in health care, what would that look like? I can tell you, it would be a lot different than it is now. How? There would be a relentless focus on creating the most reliable, error-free and efficient health care processes (the processes you are in related to your health status) as humanly and technologically possible. It isn’t that way now.
Here are some reasons:
Safety is one step away from the worker
“One step away” means, for the vast majority of safety failure events, it is the patient (you), not the “caregiver” that gets harmed. This is very, very different than other industries where, if there is a safety failure event, the worker gets harmed (maybe solely or along with customers). Examples:
In a chemical engineering company, if there is an explosion because two gases or liquids are accidentally mixed together, it’s the workers who get killed or maimed.
In the nuclear energy industry, if there is a sudden nuclear facility meltdown, the workers are among the dead and harmed (e.g., Fukushima)
In the airline industry, if the plane goes down, the pilots and flight attendants are killed and harmed along with the passengers.
In the construction industry, if there is a construction accident, it’s the workers who are killed or maimed.
In the coal mining industry, if there is a mine explosion or collapse, it’s the miners who get killed or maimed.
So you see placards in these places of work that say something like: “264 days without an accident” or “307 days without a worker’s compensation claim”
In health care, it would be seconds, not days between defects harming patients. These are called Adverse Events. The main reason being, 99% of the time, it is the patient who is killed or injured/harmed, not the worker. The staff has no personal “skin in the game”. You are likely to be much more diligent to prevent a harm event if you are at risk of being killed or harmed.
Now, there are some instances where health care staff are personally at risk. It is usually related to getting an infectious disease, like HIV. In these cases, there are some pretty good risk avoidance devices and attempts at procedures, like Universal Precautions (gown and glove before doing certain things) and IV catheters and syringes that have been engineered to prevent a staffer from sticking themselves with a needle.
These, worker related events, are much simpler problems to address than the complex nature of the multiple exposures a patient gets when they are in the health care system. And their number of worker events is miniscule compared to patient related adverse events. Examples:
The patient is the one who loses their good leg when a surgeon cuts off the wrong leg.
The patient is the one who is harmed when a sponge or instrument is left in their body during a surgery.
The patient is the one who is killed or harmed when they get an overdose of a medication or the wrong medication
The patient is the one who is harmed when a patient doesn’t get what they need or they are misdiagnosed or their test diagnosing a lethal disease gets lost.
In all of the above, the worker is unaffected. Remember the story in my post about Patient Safety? The child died. The staff lived and were unharmed.
In my experience, while trying to get health care systems to be relentless about how they actually deliver the care, this is what gets in the way. The worker isn’t harmed. Remember the COO of a system saying he didn’t think anything had to be done urgently to address patient safety because the errors had been going on for a long time? He wasn’t the one affected by adverse events. I’m betting you wouldn’t have said something like that, since you’re the one who would get killed or harmed.
The funny (or sad?) thing is, you only need a few mortal (or not even mortal) events in other industries to get the whole nation up in arms about a company (not even the whole industry). Remember when Ford Explorers were rolling over, with people killed? How about the Takata airbags (they are going bankrupt, I read)? How about Chipotle and the diarrhea (they haven’t recovered from that yet)? The Chevy Cruze ignition switch problem killing some people? Remember the national outrage about those? Chevy had to stop selling Cruze’s until they fixed the ignition switches.
There were less than 25 people killed in each of these cases. In health care, in hospitals alone, there are 210,000 people A YEAR dying of process errors. (“A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care, John T. James, PhD.;J Patient Saf & Volume 9, Number 3, September 2013)
That’s 575 people A DAY!! A Southwest Airlines 737 jetliner holds 143 people. That 273 people dying a day is the equivalent of four 737’s crashing a day. (Who thinks Southwest Airlines would still be in business if four of their 737’s crashed per day?) With no significant reduction in 15 years! And that’s only DEATHS in the hospitals. According to an article in the September 18, 2013 in BMJ Quality & Safety, 43 million people are injured worldwide each year due to unsafe medical care!!!
Here’s an analysis done on patients in US Hospitals on the prevalence of adverse events (“‘Global Trigger Tool’ ShowsThat Adverse Events In Hospitals May Be Ten Times Greater Than Previously Measured”; David C. Classen et al; Health Affairs, April 2011 30:4):
“Overall, adverse events occurred in 33.2 percent of hospital admissions (range: 29–36 percent) or 91 events per 1,000 patient days (range: 89–106). Some patients experienced more than one adverse event; the overall rate was 49 events per 100 admissions (range: 43–56).”
That means 49% of hospital admissions have an adverse event. And it’s not piquing anyone in the US or in heath care’s sensibilities.
Conclusion: The fact that it is the patient and not the worker who is at risk for the vast majority of deaths and harms in health care from errors and defects is a hindrance to creating reliable, error-free health care processes. The worker is one step away, not at risk.
Reliability is cultural; health care doesn’t have that culture
Even though the tools are available to create reliable processes in health care, the culture must propel that. Here are excerpts from the AHRQ treatise on reliability, “Becoming a Highly Reliable Organization”, 2008:
“At the core of high reliability organizations (HROs) are five key concepts, which we believe are essential for any improvement initiative to succeed:
- Sensitivity to operations. Preserving constant awareness by leaders and staff of the state of the systems and processes that affect patient care. This awareness is key to noting risks and preventing them.
- Reluctance to simplify. Simple processes are good, but simplistic explanations for why things work or fail are risky. Avoiding overly simple explanations of failure (unqualified staff, inadequate training, communication failure, etc.) is essential in order to understand the true reasons patients are placed at risk.
- Preoccupation with failure. When near-misses occur, these are viewed as evidence of systems that should be improved to reduce potential harm to patients. Rather than viewing near-misses as proof that the system has effective safeguards, they are viewed as symptomatic of areas in need of more attention.
- Deference to expertise. If leaders and supervisors are not willing to listen and respond to the insights of staff who know how processes really work and the risks patients really face, you will not have a culture in which high reliability is possible.
- Resilience. Leaders and staff need to be trained and prepared to know how to respond when system failures do occur.”
None of the above bullet points have anything to do with tools (like The Improvement Model, FOCU-PDCA, Lean Six Sigma). They all relate to what should be in the hearts and minds of health care leaders, managers and staff. Unfortunately, in health care, these things are not. The “corporate” leaders are preoccupied with Profit and Growth, the managers are executing tasks, the line staff are executing tasks, the providers are looking at individual patient issues, patient by patient (myopic view of the system).
I actually presented a synopsis of this AHRQ treatise to the board of a large physician group, hoping to gain some motivation from the group to start a cultural shift toward reliabilty. The comments from the meeting evaluation went something like this,” I don’t know how this pertains to me”. Enough said.
It turns out, even if you, as an individual, have the predispositions listed by AHRQ above, they are quickly suppressed by the leaders, managers, and the systems in health care. You generally “give up” as no one listens; no one in authority is willing to change their paradigm. You get worn down. You have no idea how many times I’ve heard that from conscientious staff and providers who decide they just don’t have the energy anymore to fight the resistance from “the higher ups” and they fall back in line with the culture of “it is what it is”, their hopes dashed. Back to “it’s just a job”.
This is different from a company like Toyota. Sakichi Toyoda was the founder of what we know as the Toyota automobile company. Sakichi actually started with loom weaving. He also came up with two basic Lean concepts: The 5 Why’s and “Pulling the Andon cord”.
[Side bar: When I started a medical director position in a relatively large hospital system in 2000, they hadn’t heard of the 5 Why’s. That’s how naïve health care was/is]
Sakichi essentially created the Toyota culture. The story goes, Sakichi had a building filled with looms on which women wove cloth. At times, a loom would mis-thread the fabric. The weaver would weave for a while without stopping and notice the mis-thread when that section was completed . She would take the fabric with the defects and throw it in piles outside the back door of the building. Sakichi noticed this and clearly saw this as waste, which was costing him money (which related to: he had to charge more per piece of fabric to make up for the waste). He got all of the weavers together and told them to watch for the mis-threading and as soon as they noticed the issue they should stop work and call for help. Then someone would help figure out what made the loom mis-thread and fix the loom. Stopping and asking for help is called Pulling the Andon cord; the 5 Why’s are used to figure out what is the root cause of the problem.
That was over 100 years ago. Reliability and minimizing waste is an inextricable part of the Toyota culture that has been there from the start. The Toyota company is one of the lowest defect companies in the world. They created Lean, which is a sophisticated defect reduction, efficiency improvement system.
The reliability mentality is absent or minimal in almost all health care systems. There are a few institutions that get close. Virginia Mason in Seattle seems to have taken Lean to heart. Intermountain Health Care in Salt Lake City UT has been using The Improvement Model for 30 years. Most health care organizations haven’t shown that they can sustain that type of improvement culture for that long. Geisinger Health Care is another that actually warrantees some surgeries. Most of their efforts are hospital based.
Unfortunately, the above organizations are outliers. And once you get out of organized systems like the above, reliability thinking basically falls off like a cliff. The systems in the ambulatory care environment are woefully unreliable.
A recent article in JAMA Surgery is telling in its title – Safety for the Surgical Patient—What Will “Move the Needle”?; JAMA Surgery July 2017 Volume 152, Number 7. They are admitting that nothing has changed in the surgery arena since the Patient Safety movement began in 1998.
The management systems in health care can’t integrate and sustain tried and true reliability systems, strategies and tactics.
This is the main reason health care systems can’t sustain process improvements intended to increase reliability in health care processes. The management system is not aligned with and the managers are not (and often can’t be) trained in process management. The management system is task oriented, the managers come from task oriented environments and jobs/positions, and task completion is valued by health care systems. Not so much for process management.
As a certified Lean Six Sigma Green Belt, I’ve either led or been a participant on many process improvement projects whose goals were to create highly reliable clinical processes. Here are the issues that inhibit successful implementation and sustainment of highly reliable processes:
Senior Leadership doesn’t understand and isn’t completely bought into what it takes to create and sustain changes that support reliability. They generally don’t put the time and attention into making things happen and holding the accountable managers accountable. They are used to something more tangible, like, re-contracting for a better price for knee replacement implants. They can see an immediate savings/ROI with that. With projects like Lean or Six Sigma projects, the improvements in reliability and quality are much less tangible and the lead-time for ROI is often 12-24 months. Sometimes, there is no financial ROI, the positive outcome is less morbidity and/or mortality.
Health Care Leaders usually have zero process improvement experience or training. Their answer usually is , “We have committees for those things”. And they never attend those. So, process improvement becomes just something going on in the organization that “those clinical and quality folks do.” Senior leaders pretty much give lip service to quality improvement. They like it, but to them, they should “just know it’s going on”. They like to brag about it at conferences. That’s about it.
Rule #1: If Senior Leadership is not 110% invested in process improvement, very little process improvement will occur, be successful, or be sustained.
Here’s an example of how leaders “support” process improvements in health care.
I’m a Medical Director at a hospital. I’m a Lean Six Sigma Green Belt helping a nurse manager get her Lean Six Sigma Green Belt. There is an issue at the hospital related to Code Blue’s and “Pre-code Blues” (when a staff person or family member notices a patient looks bad but hasn’t coded). There are too many. The hospital has a “Rapid Response Team” (another waste of money) but they haven’t tracked any KPI’s (Key Performance Indicators) to say they are at all effective.
We used the nurse manager’s floor for the “Beta” project. The nurse manager identified a team, which included a person from every job position on the floor and a hospitalist physician. We met every Wednesday at lunch time in their staff room for six months. The main assessment findings were, there was no standardization of anything related to “periodically assessing patients” including when to escalate. No standard forms, no standard process, no standard communication, no standard “triggers” (when to call the charge nurse or Rapid Response Team), no standard time sequences. Nothing standardized. Each staff person did what they did according to the way they wanted.
The team standardized everything. New standard forms for documenting vital signs. Clear triggers for Nurse Techs to call nurses and within a specified time box. Etc. The KPI for the project was unexpected transfers to the ICU for worsening clinical condition. These fell 43% and sustained there for a full year while I monitored the process.
Now, I had to calculate an ROI, because, if I couldn’t get a positive ROI, we couldn’t implement these changes in any other hospital floor. That was what the leadership valued over everything else, an ROI.
I had to partner with a finance manager to calculate the ROI (Oops, here comes trouble!) When we did the ROI, for one year for one hospital floor, the project saved $750,000 in avoided ICU costs, including shorter lengths of stay in the hospital since the patients in the 43% didn’t spend any extra days in an ICU. I thought, “This is great!” But, not so fast. The finance manager said,” Wait, look at this line item here on the financial analysis.” She pointed to a negative $50,000. I said, “What’s that?” She said, “That’s the impact to the hospital’s bottom line. (Recall the Studer paragraph and bottom line.) That’s the ROI to the hospital.
It turned out, the ICU days the transferred patients were using, when they had to get transferred there, had a higher contribution margin (the net a hospital makes) than a regular floor bed. For the hospital, the project reduced their revenue, hence the negative number.
So, I said, “But the patients and the payers are spending $750,000 less a year, we’re making care more affordable.” She said, “We’re not concerned with what others are saving. We don’t know what they do with their savings. We don’t get any of it. You can’t implement this anywhere else in the hospital”. I said, “But, the patients in the 43% have less morbidity. They are healthier! Doesn’t that mean anything?” She said, “Sorry, that doesn’t count with us. You have to produce the money to spread it.”
Me being a person who doesn’t quit, I started thinking about it. What came to mind was, if we weren’t transferring patients to the ICU, then the ICU has more capacity (my Lean Six Sigma mind kicked in). I had calculated the “number of ICU days avoided” as part of my dashboard. I went to the Bed Management (the department that accepts transfers from smaller hospitals and doctor offices) director and asked what the demand was for external ICU admissions and how many did we decline in the last 12 months. He told me they declined 1200! That demand was way higher than the capacity we generated, so, I could count every avoided ICU transfer day in a revised financial analysis. And, on top of that, a transfer to the ICU from outside the hospital had a higher contribution margin than a transfer from the floors. I met with the Finance manager again and had her include this in the calculations. It came out to a positive $250,000! We spent the next year spreading the standard work.
But you can see what’s important to the leadership. Not your health status. And not really the reliability of the process, just the money saved.
The health care management systems and their upper managers do not know how and won’t accept doing what it really takes to implement and sustain a process improvement. Health care leaders think you do a project for, say, three months, re-design a process, do a show and tell at the completion of the project and hand off the newly designed process to the manager of the department and move on to the next area. They think that the manager and staff can execute the tasks in the new process flawlessly at that point in time. Spending more time on that is a waste of time. (As a matter of fact, some senior leaders think the team process for creating the new improved clinical or business process is wasteful. I’ve actually been at meetings where the senior leaders bemoan the fact that the staff and managers are spending part of their “paid time” “sitting in a conference room”. They think that is so wasteful they calculate the cost of the staff’s salaries spent in improvement activities and call it a waste of money. They don’t get the fact that the people doing the work usually come up with the best ideas of how to fix the processes. They’d rather pay a consultant to come in and just tell the staff what to do (just give them the tasks)).
In true process improvement cultures, they understand that, for up to six months after a significant process improvement, the managers of the work floor should spend 50-75% of their time on the work floor auditing what the staff are doing and encouraging them to keep doing what was implemented during the project. This “habituates” the staff to the new way. If you don’t do this, the staff (and the manager) regress back to the “old way”. In the Toyota Production System, this is called “standing in the Ohno circle”.
The other thing is, managing a process is very different than monitoring task completion. There is always a “dashboard” of Key Performance Indicators (KPI) that have to be measured and monitored by the manager. If a KPI performance degrades below a pre-set value, the manager is supposed to take action to get the KPI back to expected performance levels. Health care managers: a. don’t prioritize the measurement system as being important, b. are distracted from monitoring or measuring because they are already overwhelmed with tasks (often meaningless, legacy tasks), which are the things they get evaluated on for raises, and c. are not adequately trained in the skills and tactics necessary to create an action plan to “revive” a degrading KPI.
Rule #2: Before embarking on process reliability improvements, make sure you have either adequately trained managers to process manage or have sufficient resources to assist managers in process management until they are proficient at it.
Rule #3: Assess and remove no or low value tasks from managers who are now accountable for process improvement and process management.
Here’s an example of how this currently plays out in health care.
I was a Medical Director of a hospital. Several years before, the Endocrinologists decided they didn’t want to be on call or take care of inpatients (See “Why Physicians Prefer Doing Shift Work”). They changed their hospital privileges to Consulting only.
Probably the most critical, emergent, serious condition in all of Endocrinology is Diabetic Ketoacidosis (DKA). The Endocrinologists had delegated care of DKA to the Intensivists (These are physicians who only take care of patients in Intensive Care Units minus Cardiac Care (the Cardiologists do that)). It’s like a Cardiologist delegating heart attacks to non-Cardiologists. I could never figure that out, why Endo’s would want to do that, but, it’s got to be “lifestyle rules, man!”. I actually had an Endocrinologist tell me he was happy that he didn’t get awakened in the middle of the night anymore with reports on blood sugar, potassium and bicarbonate readings. I seriously don’t get it.
I have to stop the story here to give you a little insight on how a lot of Specialists think. As a Primary Care Physician, I saw this a lot and had to challenge Specialists about the following phenomenon. Now, Specialists are really smart people. At the same time, they are only generally knowledgeable about the little stripe of Medicine in which they were trained. And they read their specialty journals, which can have very early experimental articles in them. Some of the articles are about experiments on animals. The Specialists reading these articles will, in their minds, extrapolate from these very early experiments to their (and often my) patients (you) without a Phase I, II, or III clinical trial. I actually had a Neurologist tell me what a goal blood sugar should be in a stroke patient because she read an article about the level of glucose in rats’ spinal fluid compared to their blood sugar. Really, a rat!
OK, so, thinking within that context, the standard of care for DKA is IV fluids, careful attention to blood sugar and blood electrolytes and an IV insulin drip. It’s been the standard of care for decades. The insulin drip allows you to adjust the dose of insulin commensurate with the blood sugar level and degree of acidosis (amount of acid in the blood). The Intensivists had decided to use a long acting sub-cutaneous insulin, like insulin glargine instead of an IV insulin drip. The package insert, Pharmaceutical company monograph and even the TV ads for the long acting insulin clearly stated “Not to be used in Diabetic Ketoacidosis”.
The Intensivists basically said they could ignore this recommendation because, theoretically (the operative word), since the long acting insulin created a steady, linear amount of insulin in the blood of ambulatory diabetics, just like the IV drip does in the hospital, they could use it in DKA, it was the same thing. ……Theoretically.
See, they were extrapolating from an ambulatory environment with a stable patient to an inpatient environment with a critically ill patient.
Well, I had to actually do a lot of Columbo work to track down the actual research that leads all long acting insulin Pharmaceutical companies to clearly state that no one should use their long acting insulin in DKA (they all say that, even the new ones like Tresiba). It turns out, a very well respected physician researcher at an academic institution started a study to see if long acting insulin (the exact one the Intensivists were using, too) could be used to treat DKA. But, I couldn’t find an article published on his findings. So, I emailed him and asked him where the article was published. His answer was, there is no article. They had to stop the study early because too many study patients experienced severe hypoglycemia (low blood sugar). They deemed long acting insulin inappropriate for treatment of DKA.
So, with this information in hand, I had to get the Vice President of Medical Affairs to tell the Intensivists to stop using the long acting insulin and use the standard of care: IV insulin. Really, they wouldn’t stop just based on the evidence.
But, now, we had to re-create a reliable process and a set of tools to make sure the DKA patients got the standard of care, since the process had deteriorated due to the physicians deviating from it for some time. We did a Lean Six Sigma project and installed the new process. For three months, I personally went to the ICU and did a chart extraction audit on every single DKA admission to the hospital. This created a score and documented any process errors that could be addressed the next day. Not that there were that many DKA admissions, about 5 a week maximum. The audit was a one sheet form with the critical steps of the process in the left column, a check mark column in the middle and a comments column on the right. Each patient took less than 10 minutes to audit. The Electronic Medical Record was incapable of doing this kind of audit, so the auditing couldn’t be automated.
The project was a success. Shorter length of stay, less hypoglycemia, etc. The project was handed off to the nurse manager of the ICU. Within a week, there were DKA patients who didn’t get an audit. I met several times with the nurse manager who bemoaned the fact that she had (guess what?) a lot of other tasks to do and it was hard to get to these medical record audits. (Ten minutes 3-5 times a week!). So, I went to the Quality Department where they had nurses called Clinical Project Coordinators (CPC), a part of whose job is to do medical record audits. I asked if they could do the audits to “relieve” the ICU nurse manager. They said they were too busy. I reported this to senior leaders. They were unwilling to order the managers in the ICU or Quality Management CPC’s to do the audits. Who knows which patient is getting what or when now.
See what I mean? No desire, no accountability, not made accountable. The current health care management system doesn’t value process management.
Quality Management Staff and Leadership must be nurses. This is another sacred cow in health care. In every health care organization I have been in when I get there, all of the positions in the Quality Management department have “Nurse required” in their job descriptions.
Now, I love nurses. They were my eyes and ears and even part of my brain when I was practicing. I have the utmost respect for nurses. At the same time, the nursing profession self selects a certain type of person. A task oriented person.
It’s just how it is. They get orders from a physician or APC and they execute the orders. This starts in nursing training. Often nurses trying to offer their opinion or expertise from the nursing point of view get shut down by physicians. Some people who go into nursing at some point (either in school or in practice) get frustrated with being relegated to “just following orders.” They leave the profession and go into some other line of work where their ideas are valued. This leaves a nursing workforce satisfied with following orders. Doing tasks.
So, the Quality Management Departments are not manned with people who have a talent for systems thinking, which is required for building and maintaining reliable work processes. If you try to get them to think from a systems perspective, the usually leave. My observance of hospital and health plan Quality Management departments is there is a lot of nurse turnover. The ones that stay are usually doing accreditation and compliance work, which is task oriented. The staff charged with planning and implementing clinical improvements don’t stay very long because they are sort of scolded for getting no results. And, other than passing regulator and accreditor site visits, their accomplishments are usually meager.
I owned Quality Management in three organizations. I actually built one from the ground up in one organization. After watching how difficult it was for nurses to drive process improvements and the frustrations they had to endure, I came to the realization that the type of person in Quality management had to change if I wanted to reach my quality and reliability goals. The first time I tried this was when I was the CMO of a health plan.
I got to this health plan just as they were re-organizing. The Quality Management department was viewed as ineffective; the health plan could never get beyond a one year NCQA status (National Committee for Quality Assurance). The best status you could get was a three year accreditation, meaning, NCQA wouldn’t come back to audit you for three years. The Director of Quality Management was being “ushered out”. I had to hire a new one. I reviewed the job description and re-wrote it so being a nurse was “preferred” but not required. This was a hard sell with the HR department, but I got it through. I started receiving applications. One was from a Respiratory Therapist (RT) manager.
I interviewed several candidates. All but the Respiratory Therapist were internal to the health plan and they were all nurses. The Respiratory Therapist not only impressed me with her systems and process improvement thinking, but she came in with a notebook detailing her self-started projects she had done in her department (on her own, not charged by hospital leadership). I knew she was the person I wanted.
Several days after my interview with the Respiratory Therapist, I got called to the health plan President’s office. He said, “I heard through the grapevine that you are seriously considering hiring a Respiratory Therapist and not a nurse to head up the Quality Management department.” I said, “Yes, she’s my front runner.” He said, “If you hire her you are likely going to have a mutiny or mass exodus of the nurses in the department. They don’t want to report to a non-nurse. They think only a nurse can head up the department. So do others in management who have complained to me.” I said, “But, I want the right person.” He said, “Look, I’m going to leave this decision up to you, but when it blows up in your face, you’ll get no support from me. You’re on your own.”
I hired the RT. I had to personally visit each of the other candidates to tell them they weren’t hired to keep the lid on things (rather than a phone call or letter/email). Some of the nurses left. We re-hired staff. Within a year, the RT Director of the Quality Management Department was the golden child of the health plan. She got Lean trained and was doing Kaizen events. We got a three-year accreditation the next year.
Health Care Leadership is preoccupied with making money and growing the business, leaving little or no time to champion reliability. Health care leaders have a choice: Spend, like, $200,000,000 on hard-wiring reliable processes of care or building a new facility somewhere where they think they can gain market share. 100% of the time, the facility wins. In the last company I worked for, the spending for improving reliability was over 100 times less than building buildings and was less than their patient satisfaction initiatives budget. I’ll bet if someone did a study about this, they would find similar numbers throughout the US health care system.
Rule #4: Don’t build another facility until the processes in your current facilities has an error and defect rate at least equivalent to Toyota.
This has never happened in the history of Medicine. Don’t you think it should? Your life depends on it!
The real bottom line is: The Health Care industry doesn’t have the will or talent to create and sustain reliable health care processes.
Now that you have the current state of affairs, stay tuned for how to accomplish the degree of reliability in health care processes you deserve but are not getting now. That’s my next post.
